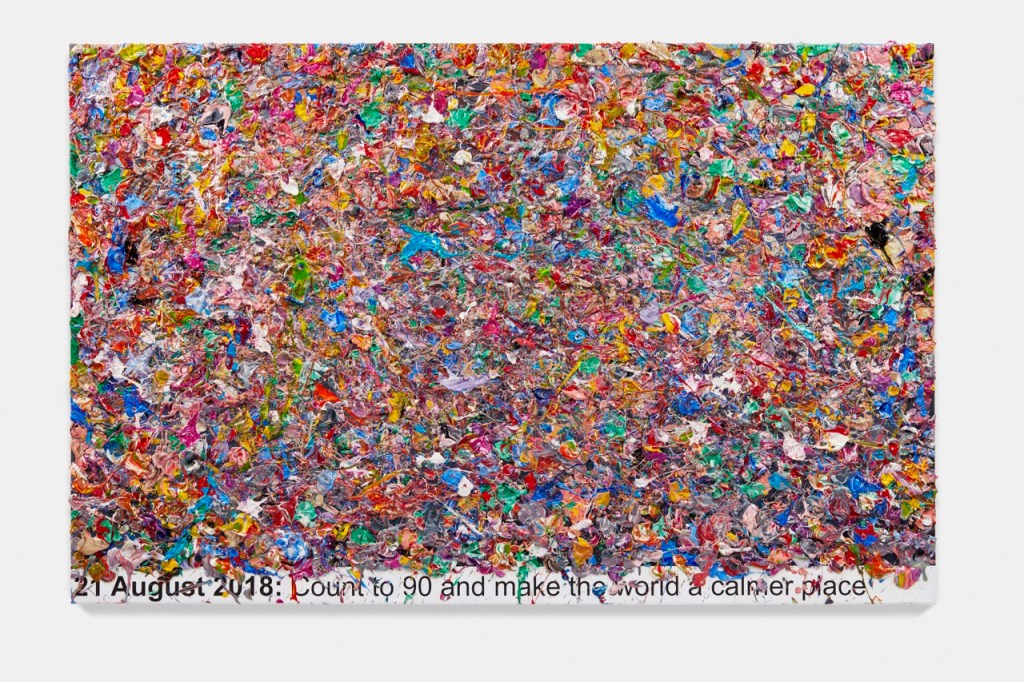
The world feels dark this week. Israel has prevented any humanitarian aid from reaching Gaza for almost 2 months. People are starving, as well as being under constant threat of bombing. Since January, 10,000 cases of acute malnutrition among children have been identified, including 1,600 cases of severe acute malnutrition. We can never say we did know. Pictures of skeletal children flood social media. “The blockade of aid is a breach of International Humanitarian Law, including Article 23 of the Fourth Geneva Convention, which mandates free passage of essential humanitarian supplies. It also violates international human rights law, including Article 11 of the International Covenant on Economic, Social and Cultural Rights, which guarantees the right to food.” Who will hold Israel accountable for these atrocities? Many countries are complicit in the genocide, including the UK, but the US is bankrolling the killing. In 2024 alone, the U.S. government sent Israel at least $17.9 billion. They could stop the horror by stopping the flow of money.