I spent this week scrolling through my news feed, watching war crimes committed by Russia in Ukraine. A hospital was just bombed. I sent more money to humanitarian organisations including Doctors of the World. Whilst it is easy to feel powerless in the face of terrible world events, there are ways we can stand in solidarity. And whilst our minds are focused on people fleeing conflict, it is a good time to consider how refugees are treated if they reach the UK and need healthcare. I was therefore pleased to be part of a panel this week, to launch the Southwark Patients not Passports campaign.
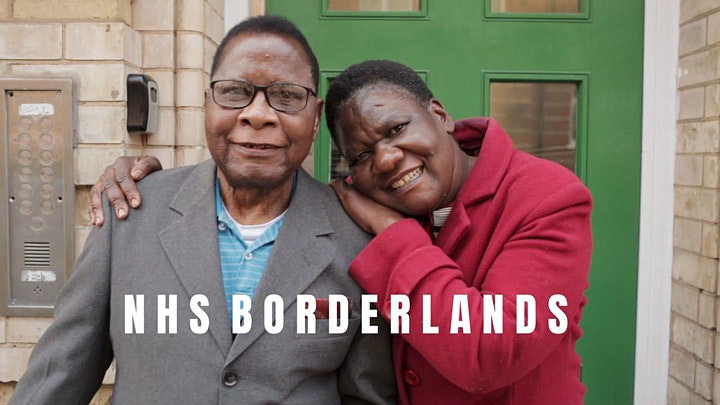
It included a screening of NHS Borderlands, an investigative documentary into the human cost of charging migrants for accessing the NHS, made by Bare Life Films. It features Angela who, after fleeing Zimbabwe in fear for her life, sought asylum in the UK where she has lived with her husband for 20 years. Following a vital hysterectomy operation Angela was – without warning – issued a bill for £8,000 by the NHS. Angela is not allowed to work and has no source of income and this bill jeopardizes her life in the UK forever. There are many stories like Angela’s, most untold and undocumented. This film shows how healthcare workers and campaigners are fighting alongside Angela to keep the border out of the NHS.
Continue reading